Incident Rehabilitation
Contents
Section 2 - EMERGENCY OPERATIONS
210.10 Incident Rehabilitation DELETE
PURPOSE:
To develop a standard for deployment of Rehab during an emergency scene or training.
PROCEDURE:
- A minimum of two firefighters are required to set up Rehab with at least one being an Autonomous Paramedic unless otherwise advised by the Incident Commander.
- Once the unit/personnel are designated as Rehab group; they are to report to the command post for briefing from the Incident Commander.
- The IC/training coordinator will establish a Rehab area, remote from the incident/training ground for the purpose of isolating personnel from the acute emotional stress of the incident/training evolution, clear of the smoke, haze or other hazardous by-products of the incident/training ground.
- Required equipment: Rehab unit with assigned equipment, salvage cover, water, ice, drinking cups, oxygen administration equipment, ECG monitor with CO monitoring capabilities, RAD 57, and basic bandaging. If possible a transport unit and stretcher with ALS equipment are also recommended.
- The Rehab group must complete a Rehab Tag on each firefighter entering Rehab.
- Personnel arriving at Rehab shall remove protective clothing to expedite the cooling process of the body.
- Members shall undergo a modified rehabilitation following the use of one 30 minute cylinder. They will not be required to enter the rehab area, but must have their pulse checked and drink one cup of water while having their cylinder changed. Once their pulse rate falls within normal limits, they will be released. If a members pulse rate continues to remain high or they present with any other abnormal signs/symptoms, they must proceed to rehab until such conditions are resolved.
- Members shall undergo rehabilitation following the use of a second 30 minute SCBA cylinder, a single 45 minute or 60 minute SCBA cylinder, or 40 minutes of intense work without an SCBA. A supervisor shall be permitted to adjust the time frames depending upon work or environmental conditions; however it is recommended that members remain in rehab for a minimum of 20 minutes
- Situations involving hazardous materials, personnel must complete the decontamination procedures prior to reporting to REHAB.
- Members entering REHAB for the first time shall rest for a minimum of 20 minutes and longer where practical.
- A supervisor shall be permitted to adjust the time frames depending upon work or environmental.
- Members shall replace calories and electrolytes as required, particularly during incidents of more than 3 hours and incidents where members are likely to be working for more than 1 hour.
- Members are encouraged to wash hands and faces whenever calorie replacement will be used.
- Initial assessments of the physical condition of each person shall be made to include pupils, skin color, skin temperature, blood pressure, and the ability to speak clearly. All inappropriate conditions shall be noted and the person shall not be allowed to return to activity until their condition has improved to within normal limits. Normal limits are defined on the Rehab Tags which are located in the Battalion and Rehab vehicles. EMS personnel shall be alert for the following:
- Personnel complaining of Chest Pain, Dizziness, Shortness of Breath, Weakness, Nausea, or Headache as these may be signs of CO poisoning.
- General complaints such as cramps, aches and pains
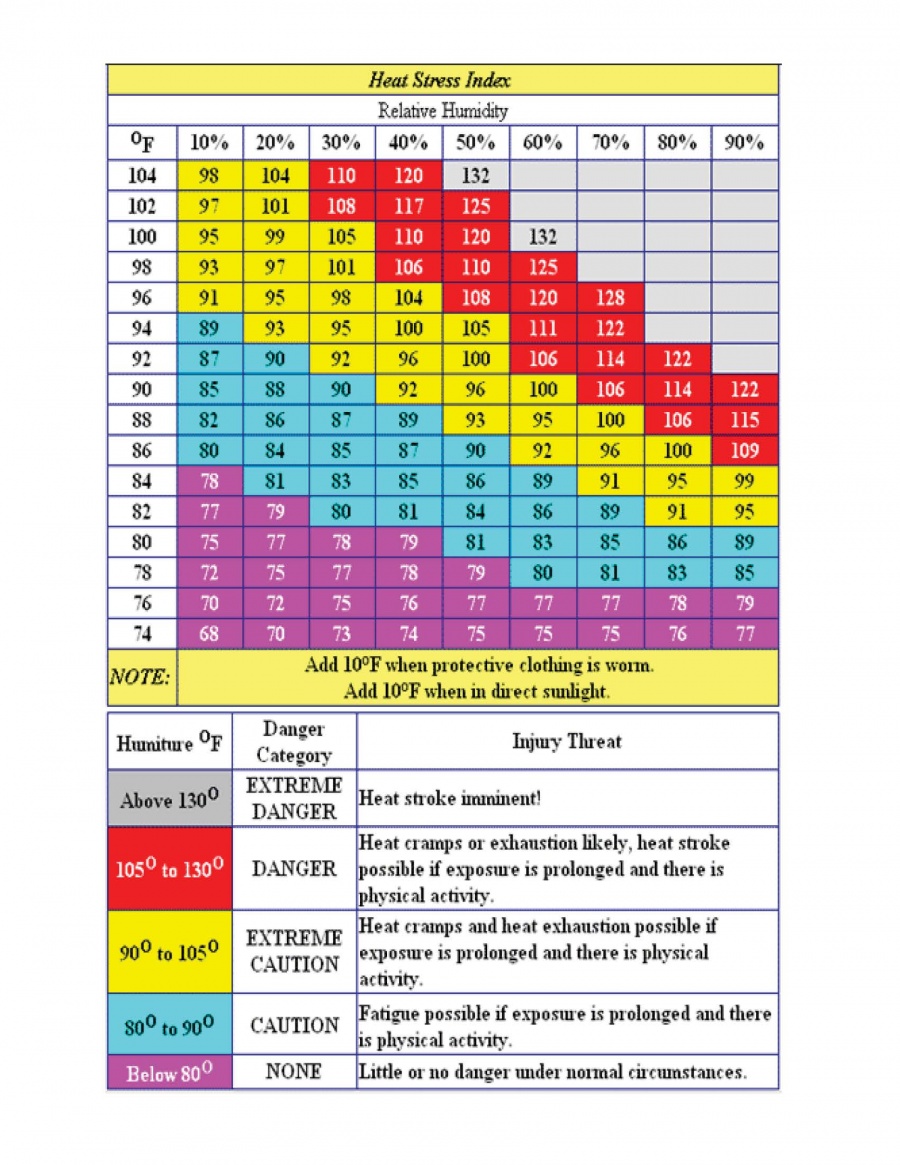
- Symptoms of heat- or cold- related stress
- Alertness and orientation to person, place, and time of members as these may be signs of CO poisoning
- Changes in gait, speech, or behavior
- Vital signs considered to be abnormal as established in protocol
- The Rehab Tags will be given to the IC or their designee once the Rehab group has been disbanded. The tags shall be scanned into the K drive and filed with the Assistant Chief of Operations.
- Firefighters should attempt to maintain proper hydration to maintain normal body function, for scheduled events, pre-hydration shall include an additional 16 oz (500 mL) of fluids within 2 hours prior to event.
Temperature. Body Temperature is a vital piece of information to assessing individuals with both heat and cold exposures. Normal core body temperature range from 98.6 to 100.6 degrees. The core body temperature (typically obtained using a rectal thermometer) provides the most accurate measurement, but is rarely feasible in the field setting. Oral measurements
are about 1 degree lower than core body temperature and tympanic measurements are about 2 degrees lower than core body temperature. Members that are hyperventilating may have a decreased oral temperature. Elevated temperature, noted by touch or measured, should alert the rehabilitation manager or EMS personnel to the possibility of heart related illness. However, given the problem of measuring devices underestimating core body temperature, it is essential that a measured temperature in the normal range not be used to exclude the possibility of heat-related problems.
Heart Rate (Pulse). Heart rate (pulse) is another critical measure used to assess health status. Normal resting heart rates range from 60 to 100 beats per minute. Under stress and exertion, the pulse rate can, and should, increase, frequently above 100 beats per minute. The level of increase depends on the amount of stress and the individual’s physical conditioning. As members report to rehabilitation after expending a significant amount of energy in stressful conditions, a pulse rate that is up to 70 percent of maximum heart rate [(220 minus age) x (0.7)] is frequently encountered. After resting in rehabilitation, the member’s heart rate should return to near normal resting rates. A fire fighter who has not achieved a heart rate of less than 100 beats per minute by the end of 20 minutes should not be released from rehabilitation, but should be further monitored, and if warranted, sent for further medical evaluation. Part of additional monitoring should include orthostatic pulse and blood pressure.
Respiratory Rate. Respiratory rate is a vital indicator used to assess health status and stress, as well as a possible indicator of exposure to other hazards. Normal respiratory rate is 12 to 20 breaths per minute. By the end of the rehabilitation period, the fire fighter should have a respiratory rate within these parameters.
Blood Pressure. Blood pressure is a critical indicator used to assess health status and stress. Blood pressure should increase as the level of physical exertion/stress increases. Blood pressures that are low, too high, or fail to return to normal levels while in rehabilitation can indicate a medical problem. For example, individuals can become hypotensive as they decompensate in their reaction to stress (e.g. heat stroke). Upon recovery during the rehabilitation, a member’s blood pressure should return to, or even be slightly lower than, their baseline. A member whose blood pressure is greater than 160 systolic and/or 100 diastolic should not be released from rehabilitation. These members should continue to be monitored and treated.
Pulse Oximetry. Pulse oximetry uses a noninvasive medical device to measure the percentage of oxyhemoglobin in blood pulsating through the network of capillaries at the probe site on a subject by utilizing a sensor attached typically to a finger, toe, or ear. It is a helpful assessment tool prior to and during oxygen administration and can be used to detect blood flow in fingers and toes. Normal SpO2 readings are between 95 and 100 percent. Readings or 91 to 94 percent reflect mild hypoxemia; 86 to 90 percent reflect moderate hypoxemia; and below 85 percent indicate sever hypoxemia. Oximetry has significant limitations and should not replace careful assessment. It can help to detect hypoxemia that is otherwise unnoticed. Black, blue, and green nail polish cause falsely low oximetry readings; when in doubt remove the nail polish
or change the probe site. Bright external lighting or sunlight can falsely lower oximetry readings. Most oximeters are unable to differentiate between oxyhemoglobin and carboxyhemoglobin (blood cells saturated with oxygen versus carbon monoxide).
CO Monitoring. Carbon monoxide is a colorless, order less gas present in every fire. Symptoms of CO poisoning are nonspecific and easy to miss. Any firefighter exposed to CO or presenting with headache, nausea, shortness of breath, or gastrointestinal symptoms at an incident where CO is present should be assessed for carbon monoxide poisoning. Carbon monoxide readily attaches to hemoglobin in the bloodstream and is measured as a percentage of carboxyhemoglobin saturation (COHb). At an incident scene, carbon monoxide can be measured with a portable exhaled breath CO monitor or a CO-oximeter (a pulse oximeter designed to measure carboxyhemoglobin).
- Initial CO Assessment Parameters
0 - 5% Considered Normal 5 - 10% Considered normal in a smoker > 10% Abnormal in any person – consider high flow oxygen > 15% Significantly abnormal in any person – treatment mandated
- CO Reassessment Parameters
0 - 5% Acceptable for return to firefighting activities if medically cleared 5 - 10% Consider high flow oxygen until < 5% regardless of symptoms > 10% Abnormal, assess for symptoms, consider high flow oxygen > 15% Significantly abnormal, treatment mandated, consider transport